Exposed Nerves: 5 Early Signs You Need Urgent Dental Treatment
By Dr Pauravi Hegde MDS, Experienced Dentist Specializing in Crafting the Perfect Smile
Table of Contents
When we talk about exposed nerves in your teeth, most people think of sudden, sharp pain—like an electric jolt—shooting through their tooth and straight to their brain. Sometimes, it’s just a quick sting when you sip a piping hot chai, and other times it feels like your entire jaw has been struck by lightning. If you’ve ever experienced that sensation, you’ll know exactly how disruptive it can be—not only to your comfort but also to your mood and your ability to perform even the simplest daily tasks.
I’ve practiced dentistry in Mumbai for years, specifically seeing patients from bustling suburbs like Sewri, Dadar, Matunga, Ghatkopar, and Antop Hill. One thing I’ve noticed is that the fast-paced city life here often forces people to ignore early warning signs of dental trouble. Patients commonly wave off minor sensitivities with a “Chalta hai” attitude, focusing on more pressing issues like packed local trains, traffic jams, or early morning schedules. But the reality is, ignoring tooth sensitivity or dull aches can lead to bigger problems—like exposed nerves that require urgent dental treatment.
In this article, I’m going to outline 5 early signs that indicate you might be dealing with an exposed nerve (or heading in that direction). I’ll also throw in personal anecdotes, prevention tips, and why immediate action is crucial—especially if you want to avoid significant pain and potential complications. Let’s dive in.
Understanding Exposed Nerves
Before jumping into the five signs, it’s important to understand what we mean by an “exposed nerve.”
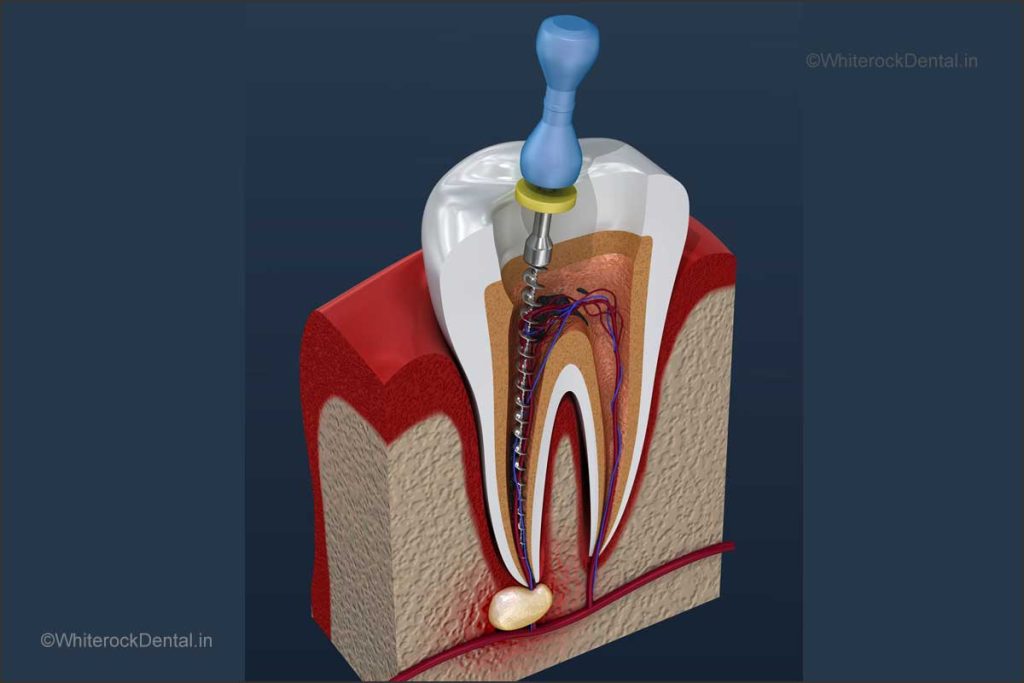
A healthy tooth is composed of multiple layers:
- Enamel – the hard, outer layer.
- Dentin – the second layer, which contains microscopic tubules leading to the pulp.
- Pulp – the soft center of the tooth that houses nerves and blood vessels.
When the protective layers (enamel and dentin) are compromised—either through tooth decay, gum recession, physical trauma, or excessive wear—the sensitive pulp becomes exposed. The result is a direct pathway for external stimuli (hot, cold, sweet, or sour) to irritate the nerve, causing sharp or lingering pain.
Common Causes of Exposed Nerves
- Poor Oral Hygiene: Skipping regular brushing or flossing can lead to plaque buildup. In time, this turns into tartar and fosters tooth decay.
- Dietary Habits: Constantly indulging in sweet or acidic foods can wear down tooth enamel. If you love those tangy chaat items in Mumbai or sugary gulab jamuns, your teeth are at higher risk.
- Teeth Grinding (Bruxism): High-stress city life can lead to unconsciously grinding your teeth at night. Over time, this persistent grinding wears away the enamel.
- Gum Recession: Gums can recede due to aggressive brushing, gum disease, or simply age. As gums pull away, the tooth’s root surface (and nerve) can be exposed.
A Personal Anecdote
Not too long ago, I treated a lovely elderly gentleman from Ghatkopar who complained of severe sensitivity. He mentioned how he’d started avoiding his favorite ice-cold kalakand because the pain was unbearable. Upon examination, I found deep gum recession around a few of his molars, which exposed the nerve-rich dentin. With a combination of periodontal treatment and careful restorations, we managed to save his teeth and bring him back to enjoying his sweet treats—albeit in moderation!
The key takeaway? Ignoring the warning signs only makes the damage worse. If you feel even a slight, consistent sensitivity or pain, it might be time to sit up and pay attention.
5 Early Signs You Need Urgent Dental Treatment
Now that you know how nerves can become exposed, let’s explore the five primary red flags you shouldn’t ignore.
1. Lingering Sensitivity to Hot, Cold, or Sweet Foods
A fleeting sensitivity—a quick zinging sensation that disappears seconds after you finish your cold coffee or hot chai—can sometimes be normal. But here’s the critical difference:
- Normal Sensitivity: You feel a mild tingle or brief jolt. It disappears almost immediately once the offending temperature or taste is gone.
- Problematic Sensitivity: The pain lingers for several seconds or minutes, and sometimes feels like a deep, throbbing ache radiating through your jaw.
When you have exposed nerves, even a mere sip of lukewarm water might set off a painful alarm. Mumbaikars who enjoy cutting chai on a street corner or who frequently indulge in falooda during hot summers often find these items triggering sensitivity. This type of lingering pain could be an early indication of nerve exposure or deep tooth decay.
Why You Shouldn’t Dismiss It
Many people rely on home remedies like rinsing with warm saltwater or popping an over-the-counter painkiller. While these measures may provide temporary relief, they fail to address the root cause. An exposed nerve worsens over time, increasing your risk for infection, abscess, or even tooth loss.
A Tip from My Practice
A young college student from Dadar once complained that she’d stopped enjoying her favorite chocolate milkshakes due to lingering sensitivity. It turned out she had a small cavity that reached closer to the nerve than expected. A simple filling and a fluoride treatment later, she was back to enjoying her sweet treats—pain-free.
2. Sharp or Radiating Pain
Sharp, shooting pain that seems to strike you out of nowhere often points to nerve involvement. Sometimes, the pain even radiates to your jaw, ear, or head, mimicking headaches or ear infections. I’ve had patients come in convinced they had an ear problem, only to discover it was actually a dental issue causing referred pain.
How It Feels
- Electric Shock Sensation: A sudden stab of pain that lasts a few seconds.
- Radiating Ache: The pain travels from your tooth to the side of your face or even down your neck.
- Triggered by Pressure: Biting down on a piece of vada pav or even lightly tapping the tooth can lead to instant pain.
Stress and Pain Connection
In a bustling city like Mumbai, stress levels run high. Stress can exacerbate any existing pain because it heightens your body’s sensitivity. Additionally, stress-related teeth grinding can expose nerve endings faster by eroding your tooth enamel.
I recall treating a professional singer from Matunga who experienced sharp pain whenever he hit certain high notes, largely due to the pressure changes in his mouth. He was initially baffled—how could singing cause tooth pain? A closer look revealed micro-fractures in his molars that were aggravating the nerves. Once we addressed those fractures and recommended a night guard to manage his bruxism, his pain vanished, and he could focus on his riyaz without grimacing.
3. Gum Inflammation or Swelling
Swollen, red, or tender gums can be a sign of several conditions, including gingivitis (early gum disease) or periodontitis (advanced gum disease). But it can also indicate that the gum is receding and exposing the tooth’s sensitive areas. If you notice:
- Persistent Bleeding: When brushing or flossing, your gums shouldn’t bleed if they’re healthy.
- Painful or Swollen Gums: This could point to an underlying infection near the nerve.
- Visible Root Surface: If you can see more of your tooth than before, your gum line might be receding.
Local Dietary Habits
We Mumbaikars love our spicy, tangy foods—everything from pani puri to schezwan dosas. Spices and acids can irritate inflamed gums further, intensifying pain and potentially speeding up gum recession if left unaddressed.
The Domino Effect
Once the gum starts to recede and the tooth’s root becomes exposed, the nerve is more vulnerable to temperature changes and bacteria. This can escalate into a severe infection if bacteria find their way into the nerve chamber. In my experience, dental infections that begin with gum issues can escalate quickly if home remedies are the only steps taken. A friend from Antop Hill tried to self-medicate for swollen gums using clove oil and turmeric pastes. While these provided temporary relief, it wasn’t long before she needed a root canal to save the tooth.
4. Visible Tooth Damage or Discoloration
Sometimes, you can actually see the signs before you feel them. If you notice:
- Chips or Cracks: Even tiny fractures can worsen with everyday chewing.
- Dark Spots or Lines: These might indicate decay leading toward the nerve.
- Exposed Dentin: This appears as a yellowish or darker layer beneath the enamel.
Accidents Happen
Mumbai is a city of hustle and bustle. Whether you’re hopping off a local train in Ghatkopar or riding a bike through Dadar’s jam-packed lanes, minor accidents—like accidentally biting down on a popcorn kernel or slipping and falling—are common. These incidents can chip or crack your tooth, giving decay and bacteria a direct path to the nerve.
Cosmetic Concerns
Some of my patients first come in because they’re concerned about a tooth looking “off” in their selfies. A bride-to-be from Matunga once noticed a dark spot on her front tooth. She was worried about how it would look in her wedding photos. Upon examination, we discovered an incipient cavity creeping close to the nerve. Had she not acted quickly, it could have turned into a painful, deep infection just before her wedding festivities. A quick filling restored her tooth both in functionality and appearance.
5. Persistent or Recurring Toothache
A toothache that goes away temporarily—only to come back with a vengeance—is a major red flag.
- Intermittent Pain: Pain might subside for a few days, fooling you into thinking the issue has resolved.
- Over-the-Counter Medications: Painkillers or topical gels can mask symptoms but do not treat the root cause.
- Impact on Daily Life: You might find it hard to concentrate at work, skip social gatherings, or avoid certain foods.
When a toothache is persistent or recurring, it often means the nerve is irritated or inflamed. This can be due to deep decay, a cracked tooth, or advanced gum disease. Painkillers may help you get through a tough day, but postponing a dental visit often leads to more complicated treatments down the line—like root canal therapy or even tooth extraction.
A Memorable Case
I remember a patient from Sewri who kept postponing her check-ups because she was juggling a busy work schedule and caring for her elderly parents. She frequently used painkillers to manage her toothache. By the time she made it to my clinic, the infection had spread to the root of multiple teeth. We had to do two root canal treatments to fully address the issue. She regretted not coming in sooner because early intervention would have meant simpler treatments and fewer appointments—which is crucial in a hectic city like ours.
Risks of Delaying Treatment
Now that we’ve covered the five key signs, let’s talk about why you should never delay treatment once these signs appear.
1. Progression of Decay and Infection
Tooth decay doesn’t stand still; it spreads. Once bacteria penetrate the enamel and dentin, they quickly move toward the pulp. When decay reaches the nerve, it can cause:
- Abscesses: A pocket of pus that forms at the root tip or in the gums.
- Severe Pain: Often throbbing, persistent, and can disrupt your sleep.
- Possible Tooth Loss: If the decay is too far gone, saving the tooth might become impossible.
For instance, a patient from Antop Hill once dismissed his toothache until he developed significant swelling. By that time, the tooth was not salvageable, and an extraction was the only option.
2. Increased Financial Burden
The longer you wait, the more complex—and expensive—your treatment becomes. A minor filling might turn into root canal treatment or even a dental implant if extraction becomes unavoidable. Factoring in the cost of multiple consultations, X-rays, medications, and follow-ups, early intervention is always the more economical route.
3. Time Constraints
In a city where time is money, multiple dental appointments can be inconvenient. Delaying treatment often means more visits to the dentist, more time off work, and more logistical hassles.
4. Potential Overall Health Complications
Oral health is linked to overall health. Infections in the mouth can lead to systemic issues if the bacteria enter your bloodstream. Conditions like diabetes, heart disease, and respiratory illnesses have been linked to poor oral health. Especially if you or a family member has a compromised immune system, an untreated dental infection can pose serious risks.
Tips for Immediate Relief and Prevention
While it’s crucial to see a dentist if you suspect any of these warning signs, there are some short-term relief measures you can take and long-term habits you can adopt to maintain a healthy smile.
1. At-Home Remedies
- Warm Saltwater Rinses: This helps reduce inflammation and can offer temporary relief. Dissolve half a teaspoon of salt in a glass of warm water and swish around the affected area.
- Cold Compress: If there’s swelling, apply a cold compress on the outside of your cheek for 10-15 minutes.
- Over-the-Counter Painkillers: While these can help with pain management, remember they’re not a cure. If pain persists for more than 24 hours, consult a dentist.
2. Good Oral Hygiene Practices
- Brush Twice a Day: Use a soft-bristled toothbrush to avoid gum damage.
- Floss or Use Interdental Cleaners: A regular flossing habit can prevent decay between the teeth, a common area for cavities to develop.
- Rinse with Mouthwash: Antibacterial mouthwashes can reduce plaque and prevent gum disease.
3. Mindful Eating Habits
- Limit Sugary and Acidic Foods: Frequent snacking on sweets like jalebis or acidic beverages like fizzy drinks can erode enamel.
- Hydrate with Water: Drinking water helps wash away food particles and bacteria.
- Balance Your Diet: Consuming a balanced diet with vitamins and minerals supports strong teeth and healthy gums.
4. Handle Stress and Bruxism
- Stress-Reduction Techniques: Yoga, meditation, or even a short evening walk can lower stress levels.
- Night Guards: If you grind your teeth at night, a custom-fitted guard can protect your enamel.
- Regular Breaks: If you work long hours on a laptop, take short breaks to relax your jaw.
When to Seek Urgent Dental Care in Mumbai
1. Recognize Emergency Symptoms
- Severe Toothache: Pain that interrupts your sleep or daily activities.
- High Fever or Swelling: Indicates a possible infection or abscess.
- Uncontrollable Bleeding: After a dental procedure or injury.
- Knocked-Out or Broken Tooth: The sooner you see a dentist, the better your chances of saving the tooth.
2. Finding the Right Dentist
In suburbs like Sewri, Dadar, Matunga, Ghatkopar, or Antop Hill, you have access to numerous dental clinics. But how do you choose?
- Check Credentials: Look for a dentist with a reputable degree and board certifications.
- Read Reviews or Ask for Recommendations: Word-of-mouth is often reliable.
- Experience and Specialization: For exposed nerves or root canal treatments, endodontic specialists can be beneficial. For those focusing on the look of their smile, choose a dentist specializing in cosmetic procedures—like me, Dr Pauravi Hegde MDS.
3. Plan Your Visit
- Appointment Scheduling: Book ahead to avoid long waiting times.
- Prepare Your Questions: List symptoms you’re experiencing and any remedies you’ve tried.
- Insurance and Payment Plans: Ask about coverage or installment options if needed.
A Personal Note: My Own Journey with Dental Anxiety
Even as a dentist, I understand the anxiety that can come with dental visits. Growing up, I had severe sensitivity in my molars, which ended up needing early fillings. I remember feeling a mix of fear and embarrassment. That memory fuels my compassion for patients who come in feeling nervous or self-conscious. My goal is always to make each visit comfortable and enlightening—helping people realize that dental care isn’t just about treating problems; it’s about fostering a healthy, confident lifestyle.
Conclusion: Don’t Let Exposed Nerves Steal Your Smile
Exposed nerves aren’t just about a bit of discomfort; they can severely impact your quality of life. From the foods you enjoy to the confidence you exude in social settings, healthy teeth and gums are a cornerstone of well-being. If you live in Sewri, Dadar, Matunga, Ghatkopar, Antop Hill, or anywhere else in Mumbai, and you’ve experienced any of the five signs discussed—lingering sensitivity, sharp or radiating pain, gum inflammation, visible damage, or a recurring toothache—don’t ignore them.
Prompt action is your best defense against escalating pain, complex procedures, and high costs. I always tell my patients: “If your tooth is talking to you in the form of pain, it’s time to listen.” Early intervention can often mean the difference between a simple filling and a more involved root canal procedure. So, schedule an appointment with a qualified dentist—and if you’re in Mumbai, I’d be delighted to help you. Your smile is worth it!


WhiteRock Dental Clinic
807 B, Lodha Supremus, New Cuffe Parade, Wadala East, Mumbai 400037, India
All content on this blog is copyright © 2024 by whiterockdental.in. Unauthorized reproduction or distribution is prohibited. For inquiries, please contact us via our website.